Pericardiocentesis
Pericardiocentesis is a critical medical procedure used to diagnose and treat the accumulation of excess fluid in the pericardial sac—the thin, protective membrane surrounding the heart. This fluid buildup, known as pericardial effusion, can compress the heart and impair its ability to pump blood effectively, leading to a potentially life-threatening condition called cardiac tamponade.
What is Pericardiocentesis?
Pericardiocentesis involves the insertion of a thin, hollow needle into the pericardial space to carefully remove the excess fluid. This procedure helps relieve pressure on the heart, improve cardiac function, and provides fluid samples for laboratory analysis to identify the underlying cause of the effusion.
Why is Pericardiocentesis Needed?
The procedure is typically recommended when a patient shows signs of pericardial effusion causing symptoms such as chest pain, difficulty breathing, low blood pressure, or rapid heart rate. Causes of pericardial effusion include infections, inflammation, cancer, trauma, or complications following heart surgery.
Timely pericardiocentesis can be lifesaving, especially in cases of cardiac tamponade, where fluid accumulation restricts heart filling and can lead to shock or cardiac arrest.
How is Pericardiocentesis Performed?
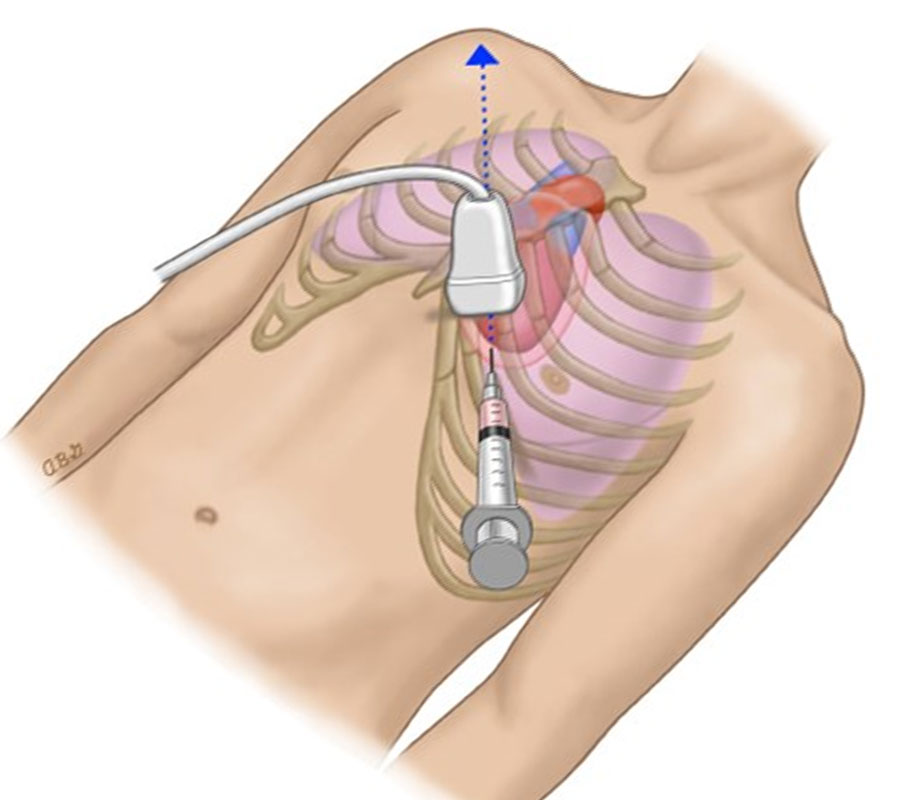
Pericardiocentesis is usually done under local anesthesia, sometimes guided by echocardiography or fluoroscopy to ensure precise needle placement and avoid complications. After sterilizing the area, the cardiologist carefully inserts the needle through the chest wall into the pericardial space. The fluid is then aspirated slowly, and in many cases, a catheter may be left in place temporarily to allow continuous drainage.
The collected fluid is sent to the lab for tests to determine infections, malignancies, or other causes, aiding in further treatment planning.
Risks and Aftercare
While pericardiocentesis is generally safe, it carries risks like bleeding, infection, puncture of the heart or nearby structures, and arrhythmias. These risks are minimized when performed by experienced cardiologists using imaging guidance.
After the procedure, patients are monitored closely for vital signs and any signs of recurrence. Follow-up imaging helps assess fluid resolution and heart function.

